- Home
- Common Foot Problems
- CMT Disease
Charcot-Marie-Tooth Disease
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Charcot-Marie-Tooth Disease (CMT), aka peroneal muscular atrophy, causes weakness and loss of sensation in the feet, legs and hands.
CMT is the most common inherited neurological disorder and affects approximately 1 in every 2,500 people.
Symptoms of Charcot-Marie-Tooth disease can include muscle weakness and loss of sensation in the extremities, such as problems with balance and coordination while walking. In more severe cases, there may also be foot deformities, scoliosis and hand and arm involvement. There can also be a significant amount of pain associated with the condition.
Whilst there is no definitive cure for Charcot-Marie-Tooth Disease, there are a number of treatment options available to reduce symptoms and slow progression of the disease.
What Is Charcot-Marie-Tooth?
Charcot-Marie-Tooth Disease is a group of inherited disorders that affect the peripheral nerves.
CMT is caused by mutations in genes that encode proteins important for the normal functioning of peripheral nerves. The most commonly affected genes are PMP22, GJB1, MPZ, and EGR2. Mutations in these genes can cause different forms of Charcot-Marie-Tooth disease and vary in their severity.
Charcot-Marie-Tooth disease was first identified in 1886 by three doctors, Jean-Marie Charcot, Pierre Marie and Howard Henry Tooth, hence the name.
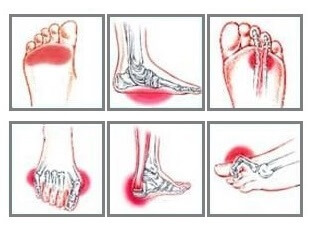
CMT develops gradually, starting with symptoms of weakness and decreased sensation in the feet which can spread progressively over time up the legs, sometimes also affecting the hands and arms. It often results in abnormalities in the shape of the foot such as high foot arches.
The severity of Charcot-Marie-Tooth Disease is determined by the gene mutation that is causing the disorder.
Charcot-Marie-Tooth Symptoms
The symptoms of Charcot-Marie-Tooth disease varying depending on the type of disease, but there are many shared characteristics including:

- Changes in Foot Position: Foot position changes are a common complication of Charcot-Marie-Tooth Disease. CMT typically results in very high foot arches but in some cases can cause flat foot arches
- Curled Toes: The position of the toes can change into a flexed position, known as hammertoe or claw toe
- Pain: may be experienced, usually associated with postural changes, nerve damage, weakness and cramp. The severity can range from mild to severe, depending on the progression of the disorder
- Muscle Weakness: Wasting of the muscles results in weakness. This starts in the feet and ankles and can gradually spread up the legs, resulting in what is referred to as an upside-down champagne bottle appearance of the legs due to muscle wasting. Weakness may also develop in the hands and forearms, making fine motor control activities like writing difficult
- Altered Sensation: Decreased or absent sensation (ability to feel touch or temperature) in the feet and hands are a common symptom of Charcot-Marie-Tooth Disease. There may also be numbness and tingling in the affected areas, such as the hands and feet.
- Cramp: Muscle cramp commonly occurs with CMT disease due to reduced muscle strength. The weakened muscles can be easily fatigued, leading to muscle cramps
- Spinal Deformity: Curvature of the spine (known as scoliosis) affects up to half of CMT disease sufferers. Spinal deformity is caused by weakened muscles in the back and abdomen, resulting in an abnormal curvature of the spine. This can lead to pain and other symptoms such as limited mobility, reduced range of motion, and difficulty walking. In severe cases, spinal deformity can cause neurologic symptoms such as numbness, tingling, and weakness in the extremities
- Difficulty Walking: Muscle weakness often leads to difficulty walking and can result in frequent trips, falls and ankle sprains due to an inability to pick the foot up effectively, known as a foot drop. Clumsiness is often one of the first signs of Charcot-Marie-Tooth disease in children
- Altered Reflexes: Common reflex changes associated with charcot-marie-tooth disease include decreased muscle contraction, diminished tendon reflexes, and absent or hyperexcitable knee jerk and ankle jerk
- CMT 3: presents during infancy, usually by the age of two resulting in floppy baby syndrome and delayed motor skills.
Symptoms of Charcot-Marie-Tooth develop gradually, usually starting during childhood and get progressively worse over time. CMT symptoms usually appear between the ages of 5 and 15 years.
Whilst CMT is a progressive disorder, in most cases, Charcot-Marie-Tooth Disease does not directly affect life expectancy. However, the severity of the condition can vary greatly and certain complications, such as foot deformities, can increase the risk of certain medical conditions, such as ulcers, that can affect a person’s life expectancy. Occasionally CMT can cause breathing problems.
What Causes Charcot-Marie-Tooth Disease?
Charcot-Marie-Tooth Disease is a type of peripheral neuropathy. Let me explain. Our bodies are made up of two nervous systems:
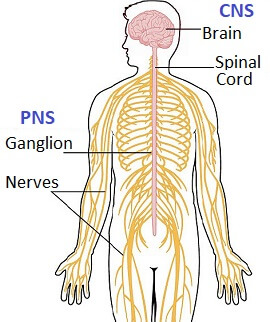
- Central Nervous System: brain and spinal cord
- Peripheral Nervous System: nerve fibres that travel round the body.
In CMT disease, there is a problem with the peripheral nervous system.
There are two types of nerve in the peripheral nervous system:
- Motor Nerves: which control movement
- Sensory Nerves: which interpret touch such as heat, cold and pressure
Our nerves work by sending messages in the form of electrical signals from the central nervous system to the rest of the body through the peripheral nervous system.
Think of them like a telephone cable. The wires inside, known as the axon, transmit the electrical signals from one place to another.
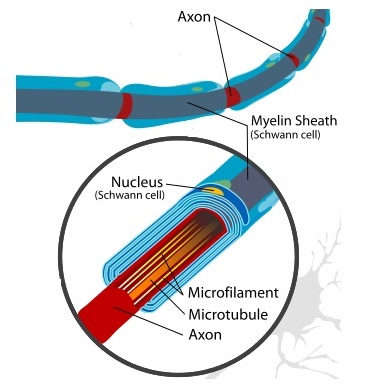
The protective outer covering, known as the myelin sheath, protects and insulates the wires from damage so the signals can transmit without interruption. It also allows signals to transmit quicker.
In Charcot-Marie-Tooth Disease, there may be a problem with:
- The Myelin Sheath: This breaks down, exposing the axon to damage, which affects the transmission of signals down the nerve
- The Axon: which reduces the strength of the electrical signals
This means that the messages being sent down the nerve to the muscles are either less frequent or less strong than usual. This affects muscle function and overtime leads to weakness.
Genetics and CMT Disease
Charcot Marie Tooth disease is caused by a problem with genes. We are made up of around 30,000 pairs of genes. For each pair, we inherit one copy from our mother and one from our father to make a pair, so we have two copies of every gene.
Charcot Marie Tooth disease can be caused by a mutation of a number of different genes. The mutation affects the production of the proteins that form the axon and myelin sheaths in the peripheral nerves. Gradually over time, the nerves degenerate, reducing their ability to transmit signals.
There are three ways that we can inherit the genetic mutations that cause Charcot Marie tooth disease:
1. Autosomal Dominant Inheritance
This is the most common cause of peroneal muscular atrophy and affects people where one parent has CMT.
Mutation of one of the inherited genes in the pair is sufficient to cause the disease. If one parent carries the mutated gene, there is a 50% chance of the disease being passed on.
2. Autosomal Recessive Inheritance
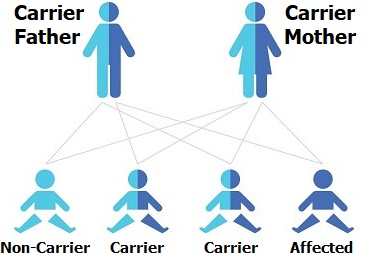
With autosomal recessive inheritance, Charcot-Marie-Tooth disease affects people who's parents are carriers of CMT gene mutations but do not have the disease themselves.
It requires a mutation of both of the copies of the gene in a pair, i.e. both parents would have to pass on affected genes.
If both parents are carriers of mutated CMT genes, there is a 50% chance of their child being a carrier (carrying one CMT gene but not displaying any symptoms), 25% chance of having CMT disease and 25% chance of inheriting two normal genes.
If only one parent had a recessive CMT gene, their child would not develop peroneal muscular atrophy but would have a 50% chance of being a carrier.
3. X-Linked Inheritance
The mutated gene is linked to the X chromosome (female), not the Y chromosome (male). Males are made up of XY chromosomes and females have XX chromosomes.
When CMT disease is linked with an X chromosome, there is a 50% chance of a mother passing the disease on. If she passes the gene on to a son, he will be symptomatic. If she passes the gene on to a daughter, she is likely to only have mild symptoms as the unaffected X chromosome tends to override the condition.
Very rarely a gene may mutate spontaneously causing peroneal muscular atrophy, rather than being passed down genetically.
Types of CMT Disease
There are five main types of Charcot-Marie-Tooth Disease:
- CMT Type 1: This is the most common type of Charcot-Marie-Tooth Disease accounting for 30% of cases. Gene duplication causes the myelin sheath to break down, known as demyelination. The body responds with a proliferation of Schwann cells which wrap around the axon resulting in remyelination. The cycle keeps repeating producing what is known as the onion bulb effect
- CMT Type 2: Results from abnormalities in the axon itself. It accounts for 20-40% of cases
- CMT Type 3: develops in infancy and results in severe demyelination and thinning of the myelin sheath. It is the most severe form of Charcot-Marie-Tooth Disease causing severe muscle wasting and weakness as well as sensory problems. It is also known as Dejerine-Sottas disease and is extremely rare
- CMT Type 4: this is a rare type of Charcot-Marie-Tooth disease that affects the myelin sheath
- CMT Type X: this is another demyelinating neuropathy caused by a mutation in the X chromosome, more commonly affecting men. It accounts for 10-20% of cases
How Is Charcot-Marie-Tooth Disease Diagnosed?
Diagnosing Charcot-Marie-Tooth Disease starts with your doctor asking you about your symptoms and any
family history of the disease. Examination will start with observation
of your foot position, testing muscle strength, reflexes and sensory
testing. They will also look for signs of enlarged nerves that can be
seen or felt through the skin.
If your doctor suspects Charcot-Marie-Tooth Disease, you will be referred to a neurologist (a specialist
doctor of the nervous system). They will carry out further tests which
may include:
1. Nerve Conduction Tests

Nerve conduction tests are used to look at the speed and strength of the signals transmitted through the peripheral nerves.
This is done using electrodes placed on the skin which produce small electric shocks to stimulate the nerves. Slow or weak signals may indicate Charcot-Marie-Tooth disease.
2. Electromyogram (EMG)
EMG's test the electrical activity at your muscles at rest and when contracting. Small needles connected to a machine are placed in your muscles. They measure the muscles electrical activity at rest and then when you try and contract the muscle.
Specific patterns of activity can be seen in some types of Charcot-Marie-Tooth disease.
3. Nerve Biopsy
If nerve conduction and EMG tests have been inconclusive, a nerve biopsy may be performed. This is when a small section of a peripheral nerve is removed under local anaesthetic and examined under a microscope for signs of Charcot-Marie-Tooth disease.
4. Gene Testing
Genetic testing from a blood sample can be used to diagnose most types of peroneal muscular atrophy, but not all genes that cause the disease have been identified yet
Charcot-Marie-Tooth Treatment
There is currently no cure for Charcot-Marie-Tooth disease, but a combination of therapy, orthotics, surgery and medication can help to reduce symptoms and slow the prgoression of the diease. Treatment for CMT Disease may include:
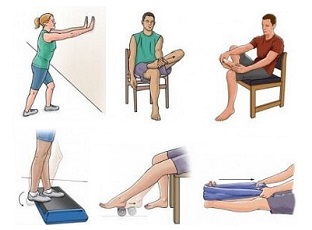
1. Physiotherapy
Rehab programmes are a vital part of peroneal muscular atrophy treatment.

Strengthening Exercises: help combat the weakness associated with the disease. Strengthening exercises for CMT are most effective when started early, before the muscles start to waste
Stretches: particularly for the calf muscles and Achilles tendon should be done daily to prevent muscle contractures from developing
General fitness programmes also help to reduce fatigue from the extra effort required for movement. Low impact activities such as cycling and swimming are recommended to limit the force put through the joints.
It can also help to work on balance and posture to prevent injuries or associated problems.
2. Occupation Therapy
This looks at ways to make your activities of daily living such as washing and dressing easier, through practical methods and using adaptive aids.
3. Orthotics
There's a huge variety of orthotics that be helpful with Charcot Marie Tooth disease, depending on your symptoms.

- Shoe Inserts: help to correct foot position such as fallen arches
- AFO: an ankle foot orthosis is particularly useful if you have a foot drop as it holds your foot in a neutral position so you aren't tripping over your toes when you walk
- Braces: ankle and knee braces can be useful for providing support and stability of the foot and leg and make activities such as walking easier
Each of these can help reduce the risk of injury for people suffering from Charcot Marie Tooth disease.
4. Painkillers
Analgesics may be prescribed to reduce pain associated with the disease. Neurotoxic drugs such as vincristine should be avoided as they can make the condition worse.
5. Activity Modification
Lifestyle modifications for Charcot-Marie-Tooth Disease can really help such as avoiding activities that may increase symptoms, e.g. running or long-distance walking.
It can really help to participate in a tailored exercise programme tailored and regular mild exercise can help maintain muscle strength, improve coordination and balance, and prevent stiffness.
Other lifestyle changes could include supportive shoes and a healthy lifestyle, including proper nutrition and regular rest.
There are a number of support groups available for people living with Charcot-Marie-Tooth disease who can provide further advice and guidance.
6. Surgery
Sometimes Charcot-Marie-Tooth disease surgery is necessary to combat structural deformities of the foot and ankle. Bone surgery such as an osteotomy or arthrodesis helps correct the shape of the foot such as realigning hammertoes, correcting severely fallen foot arches or fusing the ankle joint for stability.
Soft tissue release is done if muscles and tendons have become too type such as plantar fascia release. Spinal surgery may be required if a scoliosis has developed.
What Else Can Help?
Exercises can make a big difference for people suffering from Charcot-Marie-Tooth disease. Exercise programmes should be carried out under the guidance of a physiotherapist, but visit the strengthening exercises and ankle stretches for some suggestions of things that might help treat peroneal muscular atrophy.
If Charcot-Marie-Tooth Disease is not sounding quite like your problem, visit the foot pain diagnosis section for help working out what is wrong, or the common foot problems section.
You may also be interested in the following articles:
- Pain On Top Of Foot
- Foot Arch Pain
- Nerve Pain In The Foot
- Foot & Ankle Stretches
- Swollen Feet & Ankles
- Foot Numbness
- Burning Foot Pain
Related Articles
References
1. Gait & Posture Journal: Evaluation of muscle strength, balance and functionality of individuals with type 2 Charcot-Marie-Tooth Disease. de França Costa IMP, Nunes PS, de Aquino Neves EL, Lima Santos Barreto LC, Garcez CA, Souza CC, Pereira Oliveira PM, Sales Ferreira LA, Brandão Lima VN, de Souza Araújo AA. 2018
2. American Journal of Human Genetics: Mutations in ATP1A1 Cause Dominant Charcot-Marie-Tooth Type 2.Lassuthova P1, Rebelo AP2, Ravenscroft G, Lamont PJ et al. American Journal of Human Genetics 2018
3. British Medical Journal Best Practice: Charcot Marie Tooth Disease. May 2018
Page Last Updated: 7th October, 2024
Next Review Due: 7th October, 2026