- Home
- Common Foot Problems
- Tarsal Tunnel Syndrome
Tarsal Tunnel Syndrome
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Tarsal Tunnel Syndrome is a painful foot condition, aka TTS or posterior tibial nerve neuralgia.
Tarsal tunnel syndrome is a nerve compression injury caused by pressure on the posterior tibial nerve and typically affects people who a lot of time on their feet, either standing, walking or running.
Anything which occupies space in the tarsal tunnel, a narrow space at the inner ankle, including cysts and swelling from ankle injuries, can compress the tibial nerve.
Tarsal tunnel syndrome causes burning, pins and needles, numbness and pain on the bottom of the foot. These symptoms may extend from the heel to the big toe and adjacent three toes.
Treatment for TTS aims to reduce foot arch pain and usually consists of rest, exercises, compression bandages and steroid injections.
What Is Tarsal Tunnel Syndrome?
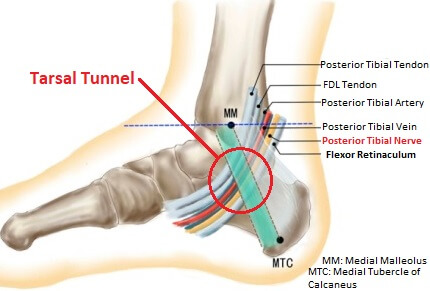
The tarsal tunnel is a narrow space found on the inner side of the ankle.
It sits just below the medial malleolus, the protruding bony lump on the inner side of the ankle, between the ankle bones and the flexor retinaculum, a strong, fibrous band that attaches to the inner ankle and heel bones.
A number of nerves, blood vessels and tendons pass through the tarsal tunnel, including the tibial nerve.
Tarsal Tunnel Syndrome develops when the tibial nerve gets squashed as it passes through the tarsal tunnel at the ankle, similar to carpal tunnel syndrome of the wrist, and is a common cause of inner foot pain.
Causes Of Tarsal Tunnel Syndrome
Tarsal tunnel syndrome can be caused by anything that increases the pressure in the tarsal tunnel. Possible causes of tarsal tunnel syndrome include:
- Space Occupying Lesions: An abnormal growth e.g. benign tumours (non-cancerous), ganglion cysts, varicose veins or neurofibroma (nerve tumour); or structural enlargement e.g. bone spurs
- Excess Fluid: swelling from an ankle injury or oedema due to fluid retention
- Altered Foot Biomechanics: Fallen foot arches place more pressure on the tibial nerve due to the altered bone positions
- Medical Conditions: e.g. diabetes, rheumatoid arthritis and thyroid disease
- Improper Footwear: Wearing shoes that are too tight increases the pressure on the tibial nerve
- Athletes: Frequent activity that places high loads through the ankle joint and thus the tarsal tunnel e.g. jumping
The flexor retinaculum cannot really stretch, so anything that takes up space in the tarsal tunnel can squash the tibial nerve. This reduces the blood flow to the nerve which leads to posterior tibial nerve neuralgia.
In approximately 30% of cases of tarsal tunnel syndrome, the cause is unknown.
Symptoms Of Posterior Tibial Neuralgia
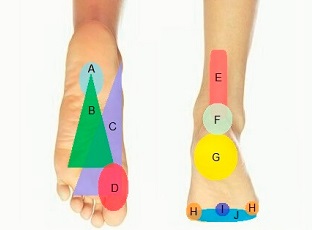
Typical symptoms of tarsal tunnel syndrome tend to be felt on the inner side of the ankle, underneath the foot and into the toes. In severe cases, symptoms may also be felt up the back of the calf to the knee.
Tarsal Tunnel Syndrome symptoms usually include:
- Foot Pain: typically a shooting or burning pain on the bottom of the foot. Pain may extend from the medial malleolus, through the heel and underneath the foot to the inner four toes. Tarsal Tunnel Syndrome pain typically eases with rest and worsens with activities such as standing, walking and driving.
- Pins & Needles and/or Numbness: Underneath the foot and into the inner first four toes
- Hot & Cold Sensation: up and down the foot
- Swelling: Around the ankle and in the foot
- Positive Tinnel’s Test: Tingling in the foot and toes with repeated tapping over the tibial nerve
The most common symptoms of tarsal tunnel syndrome are burning, numbness or tingling in the foot and/or ankle. It may also cause pain, weakness, cramping, or a feeling of heaviness in the foot. Some people may have difficulty walking due to the discomfort.
How Do You Treat Tarsal Tunnel Syndrome?
Effective treatment for tarsal tunnel syndrome typically comprises some or all of the following:
1. R.I.C.E
RICE is the best place to start with tarsal tunnel syndrome treatment.
- Rest: Avoid activities which increase your symptoms. This helps to reduce pressure on the nerve and allow it to heal. It doesn’t mean you need to take to your bed, but try to reduce how much time you are on your feet
- Ice: Regularly applying ice to the inner ankle can help to reduce pain and inflammation from tarsal tunnel syndrome. Ice should only be applied for 10 minutes at a time or else there is a risk of further injury – visit the ice therapy section to find out more
- Compression: Wearing tubigrip compression bandage can really help to reduce swelling around the ankle which in turn reduces the pressure on the nerve
- Elevation: Resting with your foot elevated (higher than your heart works best) is a great way to reduce swelling in the ankle and thus reduce the symptoms of tarsal tunnel syndrome
2. Shoe Orthotics

Wearing supportive shoes or specially designed inserts for your shoes can help to improve foot alignment by supporting the foot arches.
This helps to prevent excess pressure through the tarsal tunnel and reduce stress on the tibial nerve.
Correcting foot position can also help to reduce strain on other parts of the body, allowing for improved posture and movement.
Orthotics also help prevent ankle rolling which reduces the risk of injury and resultant swelling in the tarsal tunnel.
3. Bracing
Wearing a specially designed ankle brace limits foot and ankle movement to help reduce pressure through the tarsal tunnel.
Foot and ankle braces also provide support and cushioning while helping to control the foot's arch.
4. Medication
Common medications used to treat tarsal tunnel syndrome include non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids to reduce inflammation, swelling, and pain.
Additionally, certain types of medications, e.g. some anti-depressants, can help block nerve conduction, reducing symptoms of tingling and numbness.
5. Exercises
Exercises are an important part of tarsal tunnel syndrome treatment and are a good way to reduce the symptoms.
Progressive stretching and strengthening exercises help the foot and ankle muscles to support the ankle joint and help improve stability and reduce pressure on the tibial nerve
Neural mobilisation exercises for the tibial nerve help to improve the integrity of the nerve.
Additionally, exercises that target calf strengthening and glute strengthening may help reduce strain on other areas of the body and thereby reduce pressure on the tibial nerve as well.
6. Physical Therapy
Physical therapy is a great way to treat tarsal tunnel syndrome. Physical therapists can prescribe exercises to help strengthen and stretch the muscles around the ankle.
They can also provide hands-on therapy such as stretching, massage, and joint mobilization techniques to reduce inflammation and help ease pain.
You may also have a course of ultrasound or acupuncture to help reduce pain, inflammation and irritation.
Physical therapists can recommend bracing, orthotics, and other strategies such as taping to help relieve symptoms.
7. Steroid Injections
Corticosteroid injections can be used to help reduce inflammation and pain associated with tarsal tunnel syndrome. Typically, a combination of local anaesthetic and corticosteroid is injected into the tarsal tunnel region of the ankle.
These injections can provide short-term relief, however, they are not recommended for long-term use as they can cause side effects. Injections should be used alongside other tarsal tunnel syndrome treatments such as exercises rather than as a stand-alone treatment.
8. Weight-Loss
Overweight or obese patients often find losing weight helps to reduce their symptoms of tarsal tunnel syndrome as there is less pressure going through the foot. Weight-loss programmes should always be discussed with your doctor prior to starting
Tarsal Tunnel Syndrome Recovery
In most cases, tarsal tunnel syndrome will resolve using a combination of the treatments we have looked at, sometimes in as little as two weeks. However, in more chronic cases, recovery may take 3-6 months.
The earlier TTS treatment is started, the quicker symptoms will resolve. If posterior tibial neuralgia is left untreated for a long time, it can cause permanent nerve damage, so early diagnosis and treatment is key.
Tarsal Tunnel Surgery
Occasionally, tarsal tunnel syndrome fails to resolve with conservative treatment. If symptoms are severe then surgery may be advised, known as Tarsal Tunnel Release or Decompression.
Tarsal Tunnel Release may be done arthroscopically (key-hole surgery), or an incision may be made around the medial malleolus. Depending on the type of surgery you have you may be given a:
Local Anaesthetic: meaning you’ll be awake but won’t be able to feel anything or
General Anaesthetic: where you are put to sleep for the duration of the surgery
Tarsal tunnel surgery typically takes up to an hour and in most cases you can go home later the same day.
What Happens During Surgery?

Surgery for tarsal tunnel syndrome is typically a minimally invasive procedure and is usually done under local anesthesia.
With tarsal tunnel decompression surgery, the surgeon starts by making an incision on the inner side of the ankle to access the compressing tissues.
The flexor retinaculum is first released (cut) and then the area is fully inspected.
Any abnormal growths e.g. cysts or scar tissue are removed and any fibrous bands that are placing pressure on the posterior tibial nerve are released.
There are three other tunnels in the area, the superior, inferior and medial calcaneal channels which may also be released if needed.
The wound is typically closed using dissolvable stitches or skin glue, which allows for natural healing and prevents the need for a second surgery to remove them. The wound will be temporarily covered with a dressing to keep the area clean and protect it from further damage.
What Should I Do After Tarsal Tunnel Surgery?
Following tarsal tunnel surgery, your foot may initially feel numb. You can get up and walk within a few hours but you may need crutches or a frame initially.
In some cases your doctor may limit the amount of weight you can take through your foot for a few days/weeks and you may be given a special boot or cast to wear.
A physical therapist will go through a range of mobility and strengthening exercises with you, and will guide you through your rehab programme. You may also have a course of hydrotherapy (aqua therapy).
After a week or two you should be walking normally without any aids, and any stitches will be removed after 2-3 weeks. At this point you can usually start driving, but you must be able to safely perform an emergency stop.
People with sedentary jobs usually return to work approximately 4 weeks after tarsal tunnel surgery, but if you have a manual job it is usually best to wait around 6 weeks.
Tarsal Tunnel Surgery has advanced recently and when all four tunnels of the medial ankle are released as part of the surgery, then there is a success rate of approximately 85-90%.
What Else Can Help?
There are a number of other conditions that cause pain on the bottom of the foot. You can find out more about these in the foot arch pain and inner foot pain sections.
Alternatively, if you don't think tarsal tunnel syndrome is your problem but you want some help working out what is causing your foot pain, visit the foot pain diagnosis section.
You may also be interested in the following articles:
- Pain On Top Of Foot
- Ball Of Foot Pain
- Outer Foot Pain
- Burning Foot Pain
- Nerve Pain In The Foot
- Foot & Ankle Stretches
- Swollen Foot Treatment
- Foot Numbness
Page Last Updated: 02/23/24
Next Review Due: 02/23/26