- Home
- Common Foot Problems
- Heel Bursitis
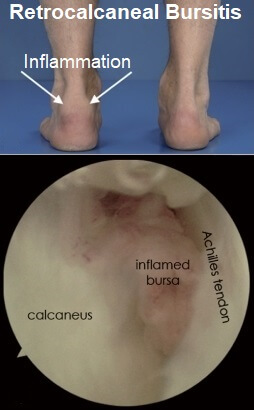
Retrocalcaneal Bursitis
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Retrocalcaneal bursitis is a common cause of heel pain due to inflammation of the bursa at the back of the heel.
Repetitive friction or pressure over the area causes irritation and inflammation of the bursa leading to pain and swelling.
Heel bursitis symptoms tend to be worse when running uphill or when standing on tiptoes.
Retrocalcaneal bursitis is often associated with heel bone spurs and is commonly misdiagnosed as Achilles tendonitis. It is the most common type of heel bursitis.
Here we will look at the common causes, symptoms, diagnosis and treatment options for retrocalcaneal bursitis and how to prevent it from coming back.
What Is Retrocalcaneal Bursitis?
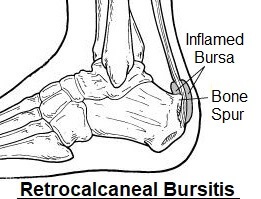
The retrocalcaneal bursa is a small fluid-filled sac that provides cushioning at the back of the heel.
It stops the Achilles tendon from rubbing on the underlying bone, allowing the tendon to glide smoothly as the foot moves up and down.
Anything which places pressure or friction on the retrocalcaneal bursa can cause it to become inflamed and fill with fluid, leading to heel bursitis. Retrocalcaneal bursitis is one of the most common causes of a soft lump on the back of the heel.
What Causes Retrocalcaneal Bursitis?
The most common causes of retrocalcaneal bursitis are:
- Activities & Over-Training: Frequent, repetitive activities such as jumping and running, particularly uphill, can irritate the bursa leading to micro-trauma and heel bursitis. Sudden increases in training or not adequately warming up before exercise increase the risk of developing retrocalcaneal bursitis.
- Wearing High Heels: Frequently wearing high heels can lead to shortening of the calf muscles and tightness in the Achilles tendon. When you then wear flat shoes or go barefoot, there is increased tension through the tendon which can cause excessive pressure on the retrocalcaneal bursa leading to inflammation.
- Wearing Ill-Fitting Shoes: Wearing poorly-fitting or tight shoes that dig in to the back of the heel can irritate the bursa. This is one of the most common causes of heel bursitis.
- Muscle Tightness: Tightness in the calf muscles can lead to increased tension on the Achilles tendon where it attaches to the heel bone. This places friction on the retrocalcaneal bursa and can cause it to become inflamed. Failing to stretch before playing sports increases the risk of retrocalcaneal bursitis.
- Bone Spur: A Haglund's Deformity is where a bony lump forms on the back of the heel in response to friction. The bony prominence rubs on the bursa leading to retrocalcaneal bursitis.
- Medical Conditions: Retrocalcaneal bursitis has be linked with certain medical conditions including gout, arthritis and fibromyalgia.
- Heel Injury: Sudden impact through the back of the heel such as a fall or being kicked can lead to inflammation of the retrocalcaneal bursa.
Heel Bursitis Symptoms
Common heel bursitis symptoms include:
- Heel Pain & Tenderness: the main symptoms of heel bursitis are pain and tenderness at the back of the heel. The pain tends to be worse when there is pressure through the back of the heel and as a result, wearing shoes is often uncomfortable. The activities that tend to cause the most pain are walking or running uphill and standing on tiptoes as in these positions the retrocalcaneal bursa gets squashed.
- Swelling: You may notice some swelling at the top part of the back of the heel due to the inflammation of the bursa forming a heel lump
- Ankle Stiffness: In some cases of retrocalcaneal bursitis, the ankle joint can become slightly stiff. This is usually due to a combination of tightness in the calf muscles and Achilles tendon, inflammation and not using the foot as normal. As a result your foot may not move around as freely or as fully.
Retrocalcaneal bursitis symptoms tend to come on gradually over time and get progressively worse, unless there has been a specific injury in which case they tend to develop rapidly.
Heel Bursitis Treatment
Treatment for retrocalcaneal bursitis looks to reduce the pain and swelling as well as the pressure on the bursa and can be divided into four stages:
Phase 1: Looks to treat the pain and inflammation
Phase 2: Looks to restore range of movement and strength at the ankle
Phase 3: Looks to restore function – getting back to the activities you love
Phase 4: Looks at prevent the recurrence of retrocalcaneal bursitis
There will be some overlap in the different phases with certain treatments being beneficial during more than one phase.
In general, the best treatments for retrocalcaneal bursitis are:
1. Rest
Rest is the best place to start with retrocalcaneal bursitis. Resting from any aggravating activities such as running or sports is essential to allow the inflammation in the heel bursa to settle down. Try to avoid any activities that exacerbate your symptoms for a few weeks. If you try to get back to activities too soon, the pain and inflammation will quickly return.
That doesn’t mean you should rest completely. Try different activities such as swimming or cycling and gentle ankle exercises to keep yourself fit and your muscles in good condition without aggravating your retrocalcaneal bursitis.
2. Regular Ice

Applying ice regularly to the back of the heel is a great treatment for heel bursitis. It helps to reduce pain and inflammation, and should be applied several times a day.
Visit the ice treatment section to find out about the best ways to apply ice and how to use it safely and effectively – it’s not as simple as just popping a bag of frozen peas on!
3. Medication
You may find it helpful to take painkillers and/or anti-inflammatories to help settle down your symptoms. Always check with your doctor before taking any medications.
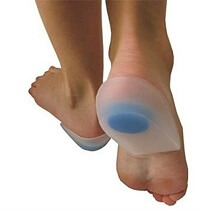
4. Orthotics
If there is tightness in the calf muscles and Achilles tendon with your heel bursitis, it can help to wear a heel wedge in your shoe. This is a simple wedge made of gel or felt to slightly raise your heel up to reduce the tension on the Achilles tendon.
In most cases, after a few weeks of regularly performing stretching exercises, you shouldn’t need to wear the heel wedge any more. Heel raises should be worn in both shoes so as not to introduce a difference in leg lengths which can lead to back and knee pain.
5. Steroid Injections
Your doctor may advise having a corticosteroid injection to treat heel bursitis. This involves injecting a solution of steroid and local anaesthetic into the bursa to help reduce the pain and inflammation.
It is important to take it easy for 3 days after an injection as it can temporarily weaken the Achilles tendon, making it prone to tearing. You can find out more about how steroid injections work on our sister site.
6. Wear Comfy Shoes
Wear soft-backed, comfortable shoes that don’t rub or place pressure over the bursa at the back of the heel. It may help to wear a shoe with a slight heel to take the tension off the Achilles tendon, but remember to do your calf stretches to alleviate any tightness.
Wearing the right shoes will help both in phase 1 of treatment to reduce pain, and also phase 4 to help reduce the risk of recurrence.
7. Foot Surgery
It is highly unlikely that you would need surgery to treat retrocalcaneal bursitis, but if symptoms have failed to resolve with other treatment methods, or there are secondary problems such as bone spurs, then it may be advised.
Surgery involves removing the retrocalcaneal bursa (known as a bursectomy) and shaving off any underlying bone spurs.
8. Calf Stretches
Stretching exercises for heel bursitis targetting the calf muscles and Achilles tendon will help to take the pressure off the retrocalcaneal bursa. Stretches are a vital part of heel bursitis bursitis treatment in phases 2 – 4 to help restore movement and function as well as reducing the chance of recurrence.
Each of the two calf muscles, gastrocnemius and soleus, should be stretched separately to ensure a full recovery. Stretches should be held for around thirty seconds each and repeated to give the muscles adequate time to stretch out.
You can find out the best ways to stretch and loads of top tips in the calf stretches section.
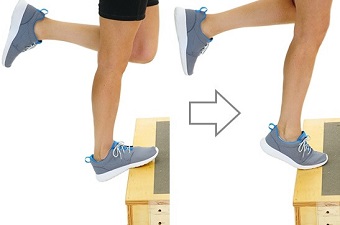
9. Exercises For Heel Bursitis
Exercises for heel bursitis to strengthen the calf and ankle muscles will help to restore function and reduce the chance of recurrent, making them suitable in phases 3 and 4 of retrocalcaneal bursitis treatment.
Strengthening exercises should not be started until the pain is under control and full range of movement at the ankle has been restored. It is important to start slowly with low numbers of repetitions and low loading exercises so as not to flare up symptoms.
Visit the strengthening exercises section for a whole range of exercises that are suitable and guidance on how to progress them.
10. Returning To Activities
Phase 3 of retrocalcaneal bursitis treatment looks at getting back to full function and being able to return to your usual activities. When returning to sports it is important, as with exercises, to wait until any pain and swelling has completely resolved, which may take a few weeks and to start slowly.
If you try and return to activities too quickly before the heel bursa has been able to fully heal, you will most likely cause a flare up of symptoms and have to start all over again.
Start by playing for shorter periods, or running shorter distances than usual and gradually build up. Ensure that you warm up and cool down before you exercise. Generally, if you overdo things, you won’t necessarily know about it immediately so don’t be tempted to rush.
A good rule to follow is the 10% rule where you increase activity levels by no more than 10% each week, be that distance or time.
Retrocalcaneal Bursitis Recovery
So how long does it take for retrocalcaneal bursitis to heal? The best way to make a full recovery from heell bursitis is to take it slowly, get the pain and inflammation under control. Then you can gradually start doing stretching and strengthening exercises, building them up appropriately.
Return to sports should not be rushed, but reintroduced slowly, gradually progressing activity levels. If you do this, you should make a full recovery within around three months.
Summary
Retrocalcaneal bursitis is a common cause of pain and swelling at the back of the heel, typically causing a soft lump on the heel. It is typically the result of over-training, tight footwear, foot abnormalities or injury causing inflammation of the heel bursa.
Treatment usually consists of a combination of activity modification, orthotics, steroid injections or medication, appropriate footwear and exercises for heel bursitis. Recovery from retrocalcaneal bursitis typically takes up to three months.
Retrocalcaneal bursitis is not the only cause of pain at the back of the heel. Other common causes include:
- Achilles Tendonitis: Inflammation and/or degeneration of the achilles tendon of the calf
- Haglund’s Deformity: Bone spur at the back of the heel
Find out about these and other different causes, including how to tell the difference between them, in the heel pain section.
You may also be interested in the following articles:
- Pain On Top Of Foot
- Foot Arch Pain
- Nerve Pain In The Foot
- Burning Foot Pain
- Foot Numbness
- Foot Lumps & Bumps
- Heel Pad Syndrome
Related Articles
Page Last Updated: 27th November, 2025
Next Review Due: 27th November, 2027