- Home
- Common Foot Problems
- Dancer's Fracture
Dancers Fracture
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

A dancers fracture is a specific type of break in one of the outer foot bones.
Sudden twisting or rolling of the foot can fracture the fifth metatarsal, the long bone on the outer side of the foot.
Dancer’s fractures are commonly associated with performers and athletes, but can affect anyone.
In most cases, these fractures can be treated with a combination of rest, immobilisation, medication, and rehab exercises, but occasionally surgery is recommended.
There are lots of different types of fifth metatarsal fractures that occur in different parts of the bone. Dancer’s fractures tend to be a diagonal break in the middle part of the metatarsal bone.
Here we will look at what a Dancers Fracture is, the common causes and symptoms, how they are diagnosed and the best treatment options.
What Is a Dancer’s Fracture?
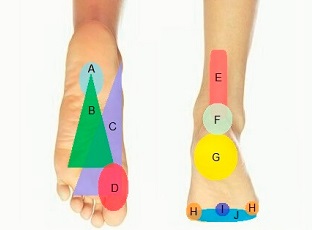
A dancer’s fracture is an oblique (diagonal) break in the shaft of the fifth metatarsal.

The fifth metatarsal is the long bone on the outer side of the foot that connects the little “pinky” toe to the mid-foot.
A dancers fracture generally affects the mid-portion of the metatarsal bone, but may extend to the head and neck.
The break usually runs diagonally along the shaft and may spiral and rotate through the bone.
In some cases, small fragments of bone will break off from the shaft, known as a comminuted fracture. There may also be some displacement, where the fractured ends of the bone move out of alignment.
This type of injury often occurs during a sudden twisting motion or an awkward landing where the foot bears an unusual force. It is frequently seen in dancers, which is how the condition got its name, but it can occur in anyone involved in high-impact activities.
There are a number of different types of fifth metatarsal fracture, all of which are slightly different:
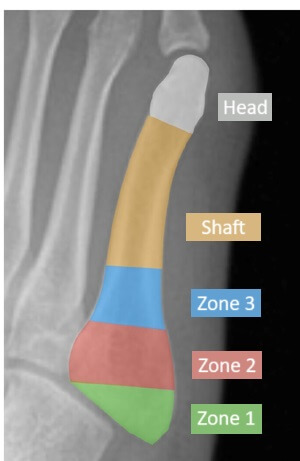
- Avulsion Fracture: Occurs at the base of the fifth metatarsal when a ligament or tendon pulls off a small piece of bone. (Zone 1)
- Jones Fracture: Occurs near the base of the fifth metatarsal but further along than an avulsion fracture. It is prone to complications due to limited blood flow in the area. (Zone 2)
- Dancer’s Fracture: Occurs along the shaft of the fifth metatarsal and typically results from acute trauma or a twisting injury. (Zone 3/Shaft)
Due to its location along the shaft, a dancer’s fracture generally has a better blood supply compared to a Jones fracture, which facilitates faster healing.
Proper treatment is critical to avoid complications such as delayed healing or chronic foot pain.
Common Causes of Dancer’s Fracture
Common causes of dancers fractures include:
- Twisting Injuries: A sudden inward twisting of the foot, particularly if the foot is plantarflexed (toes pointing down) can cause the shaft of the fifth metatarsal to fracture. This is common in dancers or other athletes during rapid directional changes.
- Awkward Landings: Landing improperly from a jump or fall, particularly on the outer edge of the foot, puts significant stress on the fifth metatarsal shaft.
- High-Impact Sports: Sports like basketball, soccer, or gymnastics often involve quick movements, pivots, or impacts that can lead to this type of fracture.
- Trauma: A direct blow to the outer side of the foot, such as from something falling onto the foot or being stepped on, can result in a dancer’s fracture.
- Overuse: While less common, repetitive stress from activities like running or dancing can weaken the bone over time, making it more susceptible to fractures.
Symptoms of Dancers Fracture
Symptoms of a dancer’s fracture may overlap with other foot injuries, so proper diagnosis is key. Common signs of dancers fractures include:
- Localized Pain: Sharp, localized outer foot pain particularly when bearing weight or moving the foot. There is usually immediate pain at the time of injury. Dancers fracture pain may feel sharp initially and then persist as a dull ache.
- Swelling and Bruising: Noticeable swelling and discoloration around the fracture site is common, extending toward the toes or ankle.
- Difficulty Walking: Pain when trying to walk or stand may make it impossible to walk without limping or favouring the unaffected foot.
- Deformity: In severe cases with significant displacement, the foot may appear misshapen or out of alignment.
- Tenderness: The fracture site is often sensitive and tender to touch
Diagnosing Dancer’s Fracture
Accurate diagnosis of a dancers fracture is essential to distinguish it from other injuries and to ensure appropriate treatment.
Your doctor will start by taking a history, asking you questions about how you injured your foot and your current symptoms. They will want to know if it is limiting any of your normal activities and what things make the pain better or worse. They will also ask about previous foot problems and any other medical conditions.
They will then carry out a physical examination of your foot, checking for pain, swelling, and tenderness along the outer side of the foot. They will look at the range of motion and strength in your foot and ankle and will have a look at your walking to determine the extent of the injury.
If they suspect a fifth metatarsal fracture, they will send you for imaging tests. X-rays are the most commonly used diagnostic tool used for dancers fractures and will confirm the location, extent and any displacement of the fracture. In some cases, you may be sent for an MRI or CT scan, usually if it is a complex fracture or there is associated soft tissue damage.
Differential Diagnosis
There are a number of other types of foot injury that present in a similar way to a dancers fracture:
- Avulsion Fracture: where a small piece of bone is pulled of the base of the metatarsal. Find Out More >
- Jones Fracture: a break in a specific part of the metatarsal that has a very poor blood supply so is commonly associated with healing issues. Find Out More >
- Stress Fracture: small cracks or breaks in the metatarsal that develop gradually, usually from repetitive overuse. Find Out More>
- Ligament Sprain: overstretching or tearing of one of the lateral ankle ligaments. Find Out More>
#CommissionEarned from Amazon on qualifying purchases
Treatment for Dancer’s Fracture
Dancers fracture treatment depends on the severity and alignment of the fracture, but in most cases the fracture is stable and can be treated conservatively
1. Immobilization
A walking boot or short-leg cast is used to stabilize the foot to allow the bone to heal in the correct position. Immobilization after a dancers fracture typically lasts 4–6 weeks until there is evidence on x-ray that the broken parts of the bone are knitting back together.
2. Relative Rest
Weight-bearing on the affected foot is often restricted initially, so you will need to use crutches. Usually you will be able to put some weight through the foot, but with severe fractures, you may need to be non-weight bearing initially.
3. Elevation

Keeping the foot elevated whenever you are sitting helps to reduce swelling.
Excess fluid is common after a fracture and it tends to pool in the foot due to gravity.
Resting with your leg elevated, ideally with your foot higher than the level of your heart will help the fluid to drain away from the foot. Either prop your leg on a pillow or use a special leg elevation cushion – these are particularly useful in bed
4. Medication
Over-the-counter pain relievers, e.g. paracetamol/acetaminophen and non-steroidal anti-inflammatories e.g. ibuprofen/Advil can help manage discomfort and swelling with a dancers fracture.
5. Gradual Weight-Bearing
Once healing progress, you can start putting more weight through your foot, and wean off the crutches. After around 6 weeks will be able to transition from your cast or walking boot to a stiff soled shoe. Always follow the advice of your doctor or physical therapist.
6. Surgical Treatment
Surgery may be necessary if the fracture is significantly displaced, does not align properly or fails to heal with conservative care. Surgical options involve internal fixation, where screws, plates, or wires are used to realign and stabilize the bone.
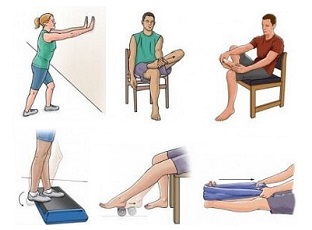
7. Rehabilitation
Physical therapy is usually recommend, with or without surgery, to regain strength and mobility in the foot after surgery. It is common for the ankle to get slightly stiff and weak following a few weeks of immobilization so strengthening exercises, ankle mobility and calf stretches are important for regain full function after a dancers fracture.
Recovery Time
Recovery from a dancer’s fracture depends on the severity of the injury and adherence to the treatment plan. A typical dancers fracture recovery time line is:
- Week 0-6: Immobilisation and restricted weight-bearing in a cast or walking boot
- Week 6-10: Gradually return to full weight-bearing and transition to stiff soled shoe, then normal shoe as pain and healing allows
- Week 10-12: Gradual return to activities e.g. dancing and sports
- Week 12-20: Gradually increase training until you return to pre-injury performance level. High-impact activities should only be resumed after clearance from a healthcare provider to avoid re-injury
It can take 6-12 months to make a full recovery from a dancers fracture, the most persistent symptom being mild ongoing swelling. Long-term issues are extremely rare.
Dancers Fracture Summary
A dancer’s fracture, an oblique break in the shaft of the fifth metatarsal, is a common foot injury caused by twisting, awkward landings, or trauma.
Symptoms include localized outer foot pain, swelling, and difficulty walking, which can be effectively diagnosed through physical examination and imaging.
In most cases, dancers fractures heal well with non-surgical treatment like immobilization and rest, but surgery may be necessary for severe or displaced fractures.
Proper treatment and rehabilitation ensure a successful recovery, allowing individuals to return to their usual activities without long-term complications. If you suspect a dancer’s fracture, seeking prompt medical attention is crucial for a smooth recovery.
You may also be interested in the following articles:
- Outer Foot Pain
- Fifth Metatarsal Fractures
- Lump On Side Of Foot
- Foot Stress Fractures
- Common Foot Injuries
- How To Reduce Foot Swelling
Related Articles
References
- Fractures Of The Distal Shaft Of The Fifth Metatarsal. "Dancer's Fracture". The American Journal Of Sports Medicine
- Fifth Metatarsal Fractures: An Update On Management, Complications, And Outcomes. European Federation Of National Associations Of Orthopaedics and Traumatology (EFORT)
- Fifth Metatarsal Fracture. PubMed Central
Page Last Updated: 2nd January, 2026
Next Review Due: 2nd January, 2028